
Blog

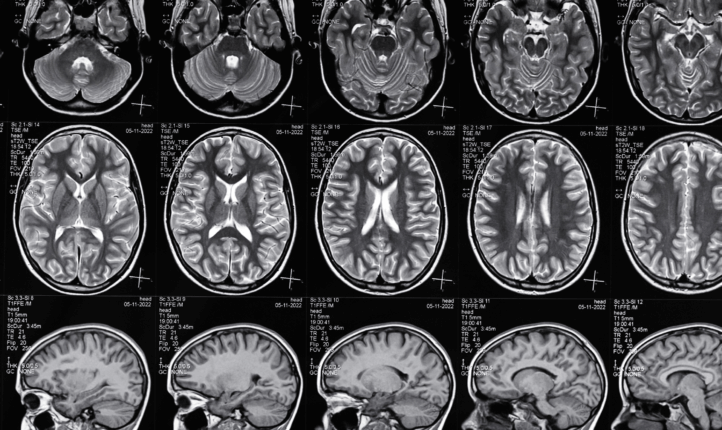
Unpacking the 2024 England Rare Disease Action Plan
Rare Disease Day 2024 (29/02/2024) saw the publication of the third England Rare Disease Action Plan. Rare conditions are individually rare but collectively common, affecting 1 in 17 people in the UK at some point in their lifetime. Almost half of the 7,000 known rare conditions are neurological. The latest action plan builds on the […]
Too costly to wait: provide care and support now and reduce the economic impact of neurological conditions
Blog by Georgina Carr, Chief Executive of The Neurological Alliance. This week new research from the Economist Unit, sponsored by Roche, found that neurological conditions cost at least £96 billion annually – and that these costs could be reduced by more than £30 billion, if care was improved, and existing options for treatment and care […]
What now for ICSs?
By Georgina Carr, Chief Executive of The Neurological Alliance I recently attended the NHS Confederation Expo, during which there was an empassioned plea from NHS England leaders to stick with Integrated Care Systems (ICSs) (including beyond the next General Election, which has to take place before January 2025). In parallel, the Government also published it’s […]

#BackThe1in6: coproduction, collaboration and campaigning to create the Neuro Taskforce
The Neurological Alliance’s coproduction group of people affected by neurological conditions has been vital to our work over the last year. They have been a driving force behind the development of the #BackThe1in6 campaign and the petition calling on all UK governments to work together to create a Neuro Taskforce to improve workforce and services […]
Recognising mental wellbeing needs: our response to the Government’s mental health and wellbeing call for evidence
Mental health and wellbeing affect us all, but don’t affect us all equally. People with neurological conditions are more likely to need mental health support than those without. While this is also true of people with other long-term health conditions, there is a unique, complex and often poorly understood interplay between the physical and the […]
Together we are stronger: coproduction and creating real impact
Our coproduction coordinator Jess Mansel describes how working with coproduction volunteers is shaping our campaign to improve neuro services. This week (4 – 9 July 2022) is Coproduction Week, and the theme is impact. We’ve been working with a coproduction group of 12 people who are affected by neurological conditions. Together, they are sharing their […]




